
Quick Links
Resources
About myRAteam
Powered By





What is Gout? | What is RA? | Causes | Symptoms | Diagnosis | Treatments | Support
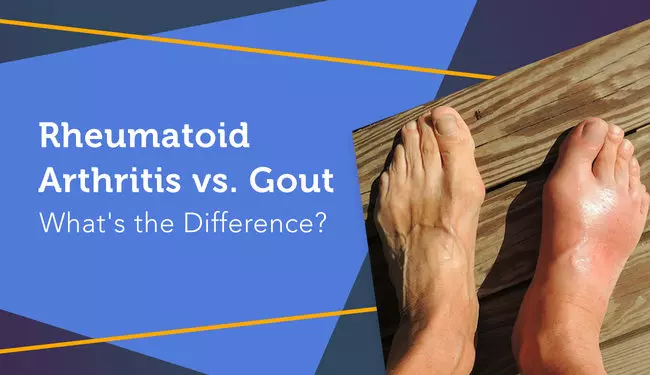
Like rheumatoid arthritis (RA), gout is a form of inflammatory arthritis. Gout and RA can cause many of the same symptoms, including joint pain, swelling, and limited range of motion. The similarities can make it difficult to determine which condition is causing your symptoms. It’s also possible to have both at the same time.
Despite their similarities, RA and gout have very different causes and often require different treatments.
Gout, also known as gouty arthritis, is a common form of inflammatory arthritis. It results from a buildup of uric acid crystals in the blood and joints. Gout typically affects one joint — often, the joint at the base of the big toe. During flares, people with gout can experience sudden, severe pain, as well as redness, tenderness, and swelling in the affected joint.
| Article: What blood tests can diagnose rheumatoid arthritis? |
Rheumatoid arthritis is an autoimmune disorder in which the immune system mistakenly attacks the joints in the same way that the immune system normally would fight viruses or bacteria. In other words, the joint damage in RA is caused by the body’s immune system. The joints of the hands, feet, wrists, elbows, ankles, and knees are usually affected. With RA, inflammation is typically symmetrical, which means it tends to be on both sides of the body.
One of the biggest differentiators between RA and gout is their cause.
Rheumatoid arthritis is an autoimmune disease. It occurs when the body’s immune system mistakenly attacks the joints. In people with RA, the body’s defenders (white blood cells and antibodies) attack the synovial membrane lining the joints. Although researchers are not sure exactly why this occurs, it is believed that both genetic and environmental factors play a role in the development of RA.
Gout occurs when an excess of uric acid builds up in the body (a condition known as hyperuricemia). The body produces uric acid when it breaks down purines — substances that occur naturally in the body, as well as in certain foods. Uric acid is normally broken down by the body and passed through the urine. Sometimes, however, the body produces too much uric acid, or the kidneys do not sufficiently process the substance, resulting in an accumulation of uric acid in the blood.
High levels of uric acid in the body can cause needle-like crystals to form in or around the joints, causing pain, swelling, and inflammation. The hyperuricemia characteristic of gout has been associated with an increased risk of cardiovascular disease and renal (kidney) disease. This risk can be concerning, as people with RA already have a higher risk of developing heart disease.
Because they are both forms of inflammatory arthritis, RA and gout share some of the same symptoms. Both can cause pain, inflammation and redness, swollen joints, and visible nodules (abnormal tissue growths). RA and gout can also cause stiffness in the affected joints, limiting the joints’ range of motion over time. These similarities may appear to make the two conditions indiscernible, but the location and onset of pain can help set them apart.
RA pain may develop slowly over time. Gout attacks, on the other hand, are often dramatic, severely painful, and quick to develop. The symptoms of gout almost always occur suddenly, in many cases developing at night. The pain of a gout attack tends to be most severe within the first 12 hours after it starts.
Many myRAteam members with gout have shared the high levels of pain the condition can cause. “I remember gout as being AGONY,” one member recalled. “You wouldn’t believe that a toe could hurt so much.” Another wrote that they “want to cut off [their] toes” when experiencing a gout attack.
Rheumatoid arthritis tends to affect similar joints on both sides of the body — if one knee joint is affected by RA, for instance, the other one will likely be affected as well. RA can affect any joint in the body, as can gout. However, the two tend to affect certain joints more frequently than others. RA often starts by affecting the small joints in the hands and feet, whereas gout typically develops in the large joint of the big toe.
MyRAteam members report experiencing gout symptoms in a variety of joints. “The gout started in my ankles,” wrote one member, who shared that their pain was particularly intense. Another member shared that they are “dealing with gout in [the] feet, ankles, and knees.” As one member admitted, “I never even thought gout occurred anywhere except for the big toe — and that’s one place I don’t have it!”
If you experience symptoms of either of these forms of arthritis, seek medical advice from your rheumatologist. They will be able to diagnose the cause of your symptoms and provide you with the right treatment.
To determine the underlying cause of joint symptoms, a doctor may perform a physical exam alongside several types of tests, including joint fluid tests, blood tests, and imaging tests.
During a physical exam, a doctor may examine your joints for signs of redness, swelling, and warmth, which may indicate inflammatory arthritis. They may also check your reflexes and the strength of your muscles.
A joint fluid test may be used to diagnose gout. This test involves drawing fluid from the affected joint and examining it under a microscope to check for uric acid crystals.
To diagnose gout, a doctor may perform a blood test to measure the levels of uric acid and creatinine (to determine how well the kidneys are functioning) in the blood. This blood test is considered a definitive test for gout, but the results can sometimes be normal during an attack of gout.
However, there is no one blood test used to diagnose RA. Instead, doctors may test for anemia and the presence of certain antibodies, including rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibodies, which may indicate that a person has RA.
Imaging tests may be used to diagnose both RA and gout. X-rays can be used to detect joint erosion (which can occur in both forms of arthritis) and rule out any other potential causes of joint inflammation. X-rays are not considered essential to diagnosing gout, as a person’s medical history, physical exam, joint fluid, and uric acid testing are often enough to identify the disease. However, X-ray images can reveal the beginnings of tophi (hard lumps or nodules from concentrated uric acid), as can dual-energy CT scans and ultrasound imaging.
Some treatments for RA and gout overlap. However, certain medications may be needed for gout to help lower the levels of uric acid in the blood.
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as Advil (ibuprofen) and aspirin, may be used to manage mild to moderate pain and inflammation in both gout and rheumatoid arthritis. Prescription NSAIDs may be used to provide stronger pain relief. If you have gout, your doctor may prescribe a higher dose of this medication during acute attacks. A lower daily dose of NSAIDs may be prescribed to help prevent future gout attacks.
Medications that reduce the levels of uric acid in the body may be prescribed to relieve the signs and symptoms of gout. Some myRAteam members take the uric acid reducer Alloprin (allopurinol). One member shared, “I take two tablets a day, and my uric acid is now within limits.” Another member mentioned that they decided to take allopurinol because they were also at risk of developing kidney stones.
If your gout does not respond to other treatments, and you have tophi, your doctor may prescribe Krystexxa (pegloticase). One member described that they receive this medication intravenously (in a vein) “every two weeks for up to six months.”
Your doctor may recommend Mitigare (colchicine), a specific type of pain reliever that reduces gout pain, during an acute gout attack. This medication may also be prescribed using a low daily dose to help prevent future attacks.
Systemic medications, which include disease-modifying antirheumatic drugs (DMARDs) and biologics, work to treat rheumatoid arthritis by slowing disease progression and preventing joint deformities. These medications treat the underlying inflammatory response that causes RA, helping to alleviate symptoms.
Corticosteroids (also called steroids) may be used in the short term to control RA and gout symptoms, including inflammation and pain. These may be taken in pill form or injected directly into the affected joint.
On myRAteam, you'll meet other people with rheumatoid arthritis and their loved ones. Here, more than 144,000 members who understand life with RA come together to share support, advice, and stories of their daily lives.
Do you have gout alongside RA? Share your experiences in the comments below, or by posting on myRAteam.
 Ariel D. Teitel, M.D., M.B.A.
is the clinical associate professor of medicine at the NYU Langone Medical Center in New York. Review provided by VeriMed Healthcare Network.
Learn more about him here.
Ariel D. Teitel, M.D., M.B.A.
is the clinical associate professor of medicine at the NYU Langone Medical Center in New York. Review provided by VeriMed Healthcare Network.
Learn more about him here.
 Victoria Menard
is a writer at MyHealthTeam.
Learn more about her here.
Victoria Menard
is a writer at MyHealthTeam.
Learn more about her here.



Become a member to get even more




A myRAteam Member
Good to know